Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Diabetes Education Intervention: Does Scholarity or Previous History of Major Adverse Cardiovascular Events Influence Its Effectiveness?
*Corresponding author:Mariana Granito, Universidade Estácio de Sá, Science and Nutrition department, Teresópolis, RJ Brazil.
Received:April 26, 2023;Published:May 04, 2023
DOI: 10.34297/AJBSR.2023.18.002507
Abstract
A patient-centered approach has been increasingly stimulated in the management of chronic diseases such as Diabetes Mellitus (DM) [1]. This approach stands for patients playing an active role in their own care and being involved in goal setting and treatment planning [2]. However, low schooling may be a barrier to this active participation and successful treatment. In fact, recent data from Brazil showed that DM mortality rate was ten times higher for people with less than eight years of study [2]. The main cause of death in patients with DM is cardiovascular disease and therapeutic efforts should aim to prevent these events. Although an acute event such as acute myocardial infarction can cause important physical, emotional and social distress, the experience can be a motivator for changes in habits and the search for information to improve self-care of the underlying disease. Education strategies as a way to improve problem-solving skills and DM self-care may be focused on individual or group basis. These strategies have already shown to positively affect glycemic control [3], although people with low schooling level have been either disadvantaged or excluded from educational proposals [4]. Also, some of these education strategies are costly, time-consuming and require a great deal of personal commitment from the health care team [3]. The purpose of this study was to evaluate and compare knowledge and attitudes of individuals with DM with and without previous history of Major Adverse Cardiovascular Events (MACE) and to determine the effectiveness of a simple and low-cost health education intervention.
Methods
This is a cross-sectional, prospective, randomized and controlled clinical study approved by the Ethics Committee of the Universidade Federal Fluminense/Hospital Universitário Antônio Pedro (CAAE: 35038014.4.0000.5243). Signed informed consent was obtained from each patient before any study procedure. During six months, every patient with DM attending the outpatient Endocrinology clinic were screened for eligibility. Inclusion criteria were: age older than 18 years; at least one year attending HUAP outpatient clinic. Pregnant women were excluded. All eligible patients willing to participate were included. Socio-demographic, clinical and laboratorial data were obtained during a small interview and from patient´s medical records. Then, patients answered two registered questionnaires (both validated and translated to Portuguese [5-7]. Diabetes Knowledge Scale Questionnaire (DKN-A) and Diabetes Attitudes Questionnaire (ATT-19) [5,6] followed by the intervention. DKN-A has 15 multiple-choice questions: One to twelve have one correct option and questions 13 to 15 have two correct options, and both should be marked for the question to be scored. A score higher than eight indicates a satisfactory knowledge level regarding DM [7]. ATT-19 has 19 questions, and it is measured through a five-point Likert scale. Alternatives reflecting a positive attitude towards DM receive higher scores (five points). A total score higher than 70 indicates positive attitude towards DM [8].
Selection of control and intervention groups was carried out in a random way. All the information of each patient was stored in envelopes, which were then sealed. The envelopes were shuffled and selected alternately for each group. The first envelope was for the intervention group. The second was for the control group, and so on. Intervention consisted in a leaflet designed by the research team, using simple language and illustrations based on authorized contents from SBD (Sociedade Brasileira de Diabetes - www.diabetes.org.br) database. Leaf let was simple and easy to read with information concerning target blood glucose levels, food groups and dietary substitutions and recognition/treatment of hypoglycemia. Leaflet was read to the patient who had the opportunity to ask questions about any topic with the research team before taking it home for further consultation. Patients who did not receive the intervention during the study (controls) remained with their usual care with medical, nursing and nutrition consultations whenever necessary. The multidisciplinary care team was blind to group allocation. All included patients were reassessed after six months with the same DKN-A and ATT19 questionnaires and clinical/ laboratorial data from medical records. At the end of the study, patients included in the control group received the same leaflet, so there was no harm to their care in relation to the patients who received the intervention.
Statistical Analysis
The statistical program SPSS version 23.0 for Windows (SPSS, Inc., Chicago, IL) was used for analysis. Numerical variables were expressed as median (p25-p75). In the descriptive analysis, categorical variables were expressed as absolute and relative values. The Kolmogorov-Smirnov normality test was performed and revealed an asymmetric distribution pattern of the numerical variables. Then non-parametric tests were used in analysis: Mann- Whitney or Kruskal Wallis tests were used to compare numerical variables between groups. Correlations between numerical variables were studied using Spearman’s correlation coefficient. A p value less than 0.05 was considered statistically significant.
Results
Participants Characteristics
During the first six months, 165 patients were included. For the present analysis, patients lacking information regarding the presence or absence of MACE were excluded, remaining 70 and 95 patients in control and intervention groups, respectively. Participants demographic and clinical characteristics are shown in Table 1. The difference in HbA1c levels between groups was clinically relevant [8.3(7.0-9.2) and8.6(7.5-9.9) vs 7.9(7.0-9.3) and 7.8(7.4-9.3) %, respectively in control (no MACE / MACE) and intervention (no MACE / MACE) groups; p=ns] although neither this nor any other variable showed statistically significant differences at baseline. For this reason, differences in pre and post-intervention HbA1c levels, DKNA and ATT-19 scores were compared as delta (difference between basal – post values, for example) between groups. A weak negative correlation was seen between basal DKNA score and age (r = -0.35; p<0.001). A negligible positive correlation was seen between basal DKNA and ATT-19 scores (r=0.15; p=0.04). No other correlations were seen between age, HbA1c levels, DKNA and ATT-19 scores.
*Note: Values presented as median (p25-p75).
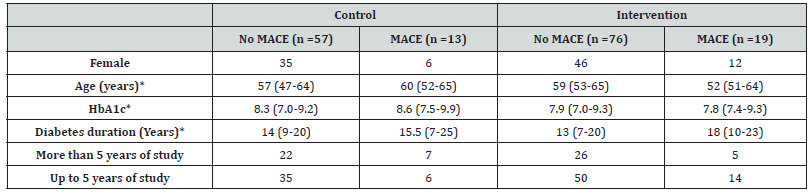
Comparison Between Patients with Up to 5 or More Years of Study
Patients with 5 or more years of study were younger [56(49.5- 63) vs 63(56.5-68.5); p=0.035]and had higher DKNA scores [10(8- 12) vs8(5-11); p=0.045] compared to patients with up to 5 years of study. No differences were seen in diabetes duration, BMI, HbA1c and ATT between groups (Table 2).
*Note: Values presented as median (p25-p75).
Comparison Between Patients with and without a Previous History of MACE
No statistically significant differences were seen in basal DKNA [10(10-12) vs 9(7-11) with and without MACE, respectively] and basal ATT-19 [70(59-77) vs 70(59-78) with and without MACE, respectively] scores between groups.
Post-Intervention Evaluation/
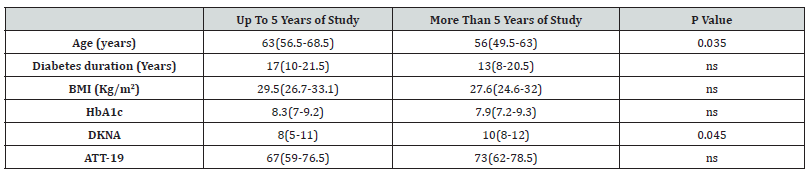
HbA1c levels, DKNA and ATT-19 scores post-intervention in each group are shown in Table 3. Difference in DKNA scores seen at the beginning of study between patients with 5 or more years of study when compared to those with up to 5 years of study was no longer present in the post-intervention evaluation [(10(9-12) vs 10(8-11); p=ns]. A higher decrease in HbA1c levels (delta HbA1c) was seen in patients with when compared to those without a previous history of MACE (p=0.037). No differences in delta DKNA or ATT-19 levels were seen between these groups (Table 3).
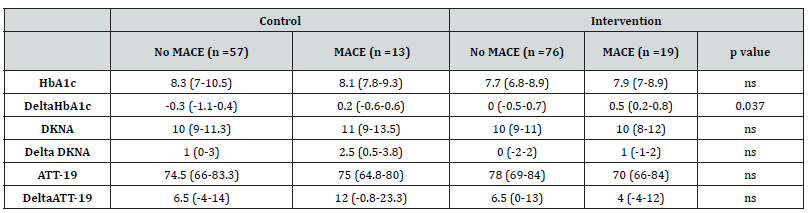
Table 3:Glycemic control, Diabetes Knowledge Scale and Diabetes Attitudes Questionnaires scores after the educational intervention.
Note: Values presented as median (p25-p75).
Discussion
This study is one of the few in correlating the profile of knowledge and attitudes about diabetes mellitus in a patient with a history of MACE and the reflect of a educational intervention. These findings are of great relevance, since patients with diabetes mellitus have >2× the risk for developing heart failure [8]. The present study included mostly elderly, undereducated patients with DM of long duration from a public University Hospital to evaluate the effectiveness of a simple and low cost diabetes education intervention. Furthermore, health costs increase with longer disease duration reaching 23% increase in those with DM for 20 years or more (Bahia, 2011). We particularly sought to assess effectiveness not only in regard of scholarity but also considering a previous history of MACE, which can be a great motivation for changing attitudes towards DM. We expected to find higher DKNA scores and lower ATT-19 scores and HbA1c levels in patients with a previous history of MACE with the reasoning that a previous cardiovascular event would have served as a motivator for knowledge acquisition and better self-care. However, neither was true and a possible explanation is that patients in this tertiary care center have long disease duration and multiple comorbidities. Moreover, even though they have not presented MACE, many patients have advanced stage microvascular complications and perhaps in this sense they behave in the same way as patients with a previous history of MACE. Regarding attitudes, failure to find different ATT-19 scores in our sample population with and without a previous history of MACE may be due to the fact that multiple factors influence attitude toward a chronic disease, such as resilience, social and cultural factors, family involvement and support. In fact, in a recently published paper, Kirchberger, et al. 2019 resilience was found to have the strongest relation with mental health-related quality of life (HRQOL) and the second strongest relation with physical HRQOL one year after an acute myocardial infarction. Finally, relevant unpublished data is that most patients have been attending our outpatient endocrinology clinic for a long time and therefore, have been receiving relevant information about their disease from the multidisciplinary care team.
Including undereducated patients in diabetes education programs is challenging. In fact, this group of patients is typically not included in clinical research trials [3-5] and previous studies showed that this specific group benefits less from these interventions [5]. However, it is very important to include these vulnerable patients, especially when we find in our sample population that patients with up to five years of study were older and had lesser DKNA scores than those with higher education. Also, a negative correlation between age and diabetes knowledge (DKNA) scores was seen and this probably is related to low schooling level in older individuals. It is heartening to see that the much-criticized government education policies from our country seem to have had some beneficial effect in recent decades, as evidenced by the higher schooling level in younger patients observed in the present study. As previously stated, it is of utmost importance not to leave the most sensitive population group, the elderly, unattended in diabetes educational programs. In this sense, a very encouraging result of the present study was that the difference in DKNA scores seen at the beginning of the study between patients with 5 or more years of study when compared to those with up to 5 years of study was no longer present in the post-intervention evaluation. This suggests that precisely these older undereducated patients benefited from this simple education intervention, matching their knowledge results (DKNA scores) with those of younger and more educated patients.
A negligible positive correlation was seen between basal DKNA and ATT-19 scores (r=0.15; p=0.04). We expected to observe a stronger correlation between these parameters, however, in addition to knowledge, other factors certainly interfere with the way the individual cope with DM. It is well described how patients endure difficulties in all bio-psycho-social-cultural aspects. This reinforces the need for a multidisciplinary team approach to help patients, including educational actions that encourage and empower patients for self-care [10]. It is important to note that in pre-intervention evaluation, a clinically relevant difference was seen in HbA1c levels between control and intervention groups. Although this was not statistically significant, we found that it could interfere with statistical analyses and decided to create a new variable that was the difference between pre- and post-intervention levels (delta). This strategy was used for HbA1c, DKNA and ATT-19 which were variables of greatest interest in the study. Also, heart failure patients with low health literacy are considered as highrisk population with poor self-care confidence and negative health outcomes and low life expectancy rates [9]. Illiteracy is present as a complicating factor in adherence to drug treatment [9], because, although patients are interested in changing life habits and follow the prescriptions, there are times when this becomes impossible, due to the inability to reading and understanding (Albuquerque G, 2016). In this sense, this health education could help the illiterate patient, since educational actions should be planned, aiming to develop attitudes and practices related to self-care, increasing their autonomy and decreasing the dependence of family members on disease control (Oliveira S, 2015), since the glycemic control in this population is poorer than the others” [10]. When we evaluated the results, we noticed that the patients showed improvement in knowledge (positive delta for the two groups analyzed). The absence of statistical difference in the scores of the questionnaires can be explained by the fact that the N studied is composed of a diabetic population and, therefore, bears a risk factor for cardiovascular disease. Another pertinent interpretation is based on the fact that in both groups the median time of illness is greater than 10 years. Thus, it can be said that such patients have been regularly monitored by a multidisciplinary team for at least 1 year, which improves their access to information and even the degree of interest in the disease.
Analyzing post-intervention data, glycemic control (HbA1c) delta (pre and post intervention) is clinically relevant. Both groups had satisfactory results of knowledge and attitudes, but only the MACE group had better glycemic controls after the intervention. It is very likely that MACE patients are more committed to putting their knowledge into practice, due to the severity of their presented complications, since the individual does not necessarily put into practice the proposed healthy habits. According to Oliveira [10] infarcted patients recognized the importance of changing lifestyle and understand that changing habits decrease the chances of having a new episode of infarction. With the emergence of restrictions, limitations and insecurity in their daily lives, patients claimed to have changed their lifestyle due to their new health condition” (Gois K, 2017). Thus, since a large part of the leaflet was prepared based on food issues, there was a significant change in the glycemic profile suggesting that a simple individual educational intervention with distribution and elucidation of an educational material can be an effective tool in the treatment. The leaflet may have helped though stimulation of good habits by these patients which reflected in improvement of glycemic control, similar to the one described by [11-14].
Conclusion
Patients with a previous history of MACE can benefit from a simple intervention, such as the distribution and explication of a leaflet associated with an elucidating conversation with a health professional, showing clinically significant improvements in your glycemic control, which is an important part of MACE prevention. Thus, this study showed that patients with little schooling had be benefited from a simple educational intervention. These are important results, since the approach of this patients is generally more difficult, and they are generally excluded from educational intervention studies because they are difficult to access. In addition, we also know that educational interventions often require a lot of time and financial resources, as well as a large health team involved. So, this paper provides an easy way to help these patients. It may increase knowledge and attitudes’ level and even help in glycemic control.
Conflict of Interest
No conflict of interest.
References
- (2019) International Diabetes Federation – IDF. Diabetes Atlas, 9th ed. Brussels.
- Stellefson M, Dipnarine K, Stopka C (2013) The Chronic Care Model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis 10: 26-28.
- Braz VN, Lopes MHBM (2018) Evaluation of mobile applications related to nutrition. Public Health Nutrition 8: 1-6.
- Campbell EM, Redman S, Moffitt PS, Sanson Fisher RW (1996) The relative effectiveness of education and behavioral instruction programs for patients with NIDDM: a randomized trial. Diabetes Educ 22(4): 379-386.
- Curcio R, Lima M, Alexandre N (2011) Instrumentos relacionados ao diabetes mellitus adaptados e validados para a cultura brasileira Rev Eletrônica Enferm 13(2): 331-337.
- Torres HC, Hortale VA, Schall VT (2005) Validação dos questionários de conhecimento (DKN-A) e atitude (ATT-19). Rev Saude Publica 39(6): 906-911.
- Beeney LJ, Dunn SM, Welch G (2001) Measurement of diabetes knowledge: the development of the DKN scales. In: Bradley C, editor. Handbook of psychology and diabetes. Amsterdam: Harwood Academic Publishers: 159-189.
- Kenny HC, Dale Abel E (2019) Cardiac adaptations to obesity, diabetes and insulin resistance. Circ Res 124(1): 121-141.
- Sany SBT, Peyman N, Zadehahmada Z, Fernsc G, Doostid H, et al (2019) Effect of educational interventions on health literacy in patients with heart failure. International Journal of Health Promotion and Education 57(1).
- Gao J, Wang J, Zheng P, Haardörfer R, Kegler MC, et al. (2013) Effects of self-care, self-efficacy, social support on glycemic control in adults with type2 diabetes. BMC Fam Pract 24(14): 66.
- Reagan L, Pereira K, Jefferson V, Evans Kreider K, Totten S, et al. (2017) Diabetes Self-management Training in a Virtual Environment. Diabetes Educ 43(4): 413-421.
- Torres HC, Pace AE, Stradioto MA (2010) Análise sociodemográfica e clínica de indivíduos com Diabetes Mellitus tipo 2 e sua relação com o autocuidado. Cogitare Enferm15(1): 48-54.
- Cortez DN, Macedo MML, Souza DAS, Santos JC, Afonso GS, et al. (2017) Evaluating the effectiveness of an empowerment program for self-care in type 2 diabetes: a cluster randomized trial. BMC Public Health 17(1): 41.
- Ricci Cabello I, Ruiz Pérez I, Rojas García A, Pastor G, Rodríguez Barranco M, et al. (2014) Characteristics and effectiveness of diabetes self- management educational programs targeted to racial/ethnic minority groups: a systematic review, meta-analysis and meta-regression. BMC Endocr Disord 14: 60.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.